Why do we almost always receive vaccines via injection? Wouldn’t a pill be much easier? It would of course, but creating an oral vaccine is anything but easy. Ground-breaking research by Professor Eric Cox and Professor Bert Devriendt (Faculty of Veterinary Medicine) may well change this.
One of the first efficient vaccines against polio was an oral vaccine. So it is quite strange that there are still only a limited number of oral vaccines available on the market. The reason for this has everything to do with our intestinal wall.
Professor Eric Cox explains: “Suppose you ingest bacteria or viruses while eating or drinking, much of them are destroyed by stomach acids and digestive juices. An oral vaccine has the same barriers, and has to pass through the intestinal wall intact enough to work.”
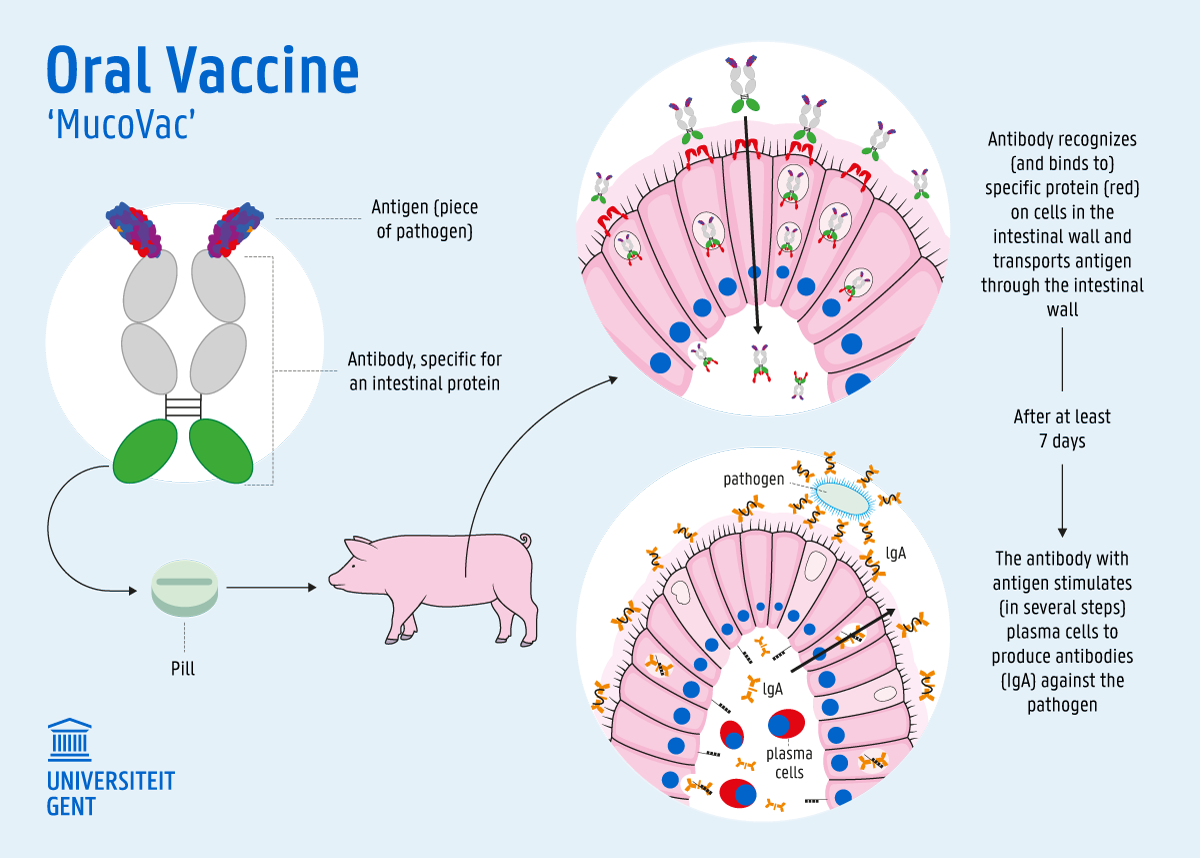
Vaccines usually work with antigens: essentially pieces of a virus or bacteria that are introduced into the body to trigger an immune response. These antigens immediately enter the blood via a shot, but via a pill they must first pass through the intestines. The gut wall is a first line of defense against foreign antigens. “So we had to find a solution to get the antigens through the intestinal wall quickly and so ‘escape’ the digestive juices.”
Groundbreaking research
The vaccination strategy developed by Professor Cox and Professor Devriendt has found a solution to this problem. Eric Cox: “Some pathogens or antigens trigger a strong immune response in the body. We discovered that they pass through the intestinal wall more easily. They do this by attaching themselves to a protein on the intestinal wall. As soon as they bind to that protein, pieces of the pathogen or antigen pass through the intestinal wall. Thereafter the immune system kicks in and you get a strong immune response. We wanted to simulate that with a vaccine by also targeting the intestinal protein. This allows the antigens to escape degradation and still provoke a fierce immune response in the body. As soon as they have passed through the intestinal wall, they are released and stimulate a specific defense of the body. In our research - we are now testing on pigs - there are no side effects for the time being.”
Eric Cox: “The oral vaccine we are developing is a vaccine that uses an antibody to feed the antigen to the immune system. No live virus or bacteria is needed, as is the case with many other vaccines. Nobody is doing this today and that is why we think we are very innovative (laughs).”
Their vaccine strategy can be used for various diseases. “If we know what the crucial protein of the pathogen is, such as the spike protein in the new coronavirus, we can link it to the same antibody and vaccinate orally.” A corona vaccine via a pill would therefore be possible in the future.
Benefits of Oral Vaccines
An oral vaccine has many advantages. Bert Devriendt: “The big advantage is that you don’t have to have an injection and won’t suffer from any side effects. This increases the willingness of people to be vaccinated. It is especially true for children.” Eric Cox adds: “In animals too, you can easily put a pill in their diet, while otherwise you would have to inject each individual animal.”
Oral vaccines can be easily transported and stored at normal refrigerator temperatures, which is convenient for logistics. But the greatest asset of an oral vaccine is that it also stops the spread of the virus or bacteria, and not just the symptoms. Bert Devriendt: “The corona vaccines that are currently under development will probably only eliminate the symptoms, but not actually prevent the spread of the virus. While the immune response that we induce with an oral vaccine also stops the spread of the germs.”
When can we expect the first oral vaccine?
With studies still ongoing, the first oral vaccine will only be on the market in 2022 at the earliest. Bert: “A trial is currently underway with pigs to determine the effectiveness of a first vaccine that we’ve developed for a common pig disease, E. coli diarrhea. We hope to know the results by the end of the year.”
Eric Cox: “The next step is to make the bridge to people. We’ll keep going with pigs at the same time. But if the first vaccine is successful, we will supplement the range with other pathogens. We want to develop a technology platform around this — we have already patented our technology — and expand it to other animal species and humans. We are working together with researchers from UZ Ghent to make the jump towards humans.”
Eric Cox: “To make companies enthusiastic about our technology, we’re distributing our research reports via Ghent University’s TechTransfer and the Provaxs consortium (for veterinary medicine). It is very important that we’re able to demonstrate that our vaccine strategy leads to protection. The proof of concept is now a priority on our to-do list.”
Confidence in their strategy is strong and ambitions are high. Eric Cox: “Together with TechTransfer, we are looking at whether we can turn our platform into a spin-off and start up our own company. This will be possible if we succeed in developing a click system by which we can quickly and easily click another antigen onto the antibodies.”
From animal to human
We are all a little bit related to pigs, and that is an advantage for the study, as it turns out. Eric Cox: “I can give you a list of about 30 pathogens that affect pigs that can also infect humans. There is a lot of similarity. We can therefore easily transfer things that we develop in the pig to humans.” He is absolutely convinced that the pig will lead to even more medical insights in humans.
Bert Devriendt: “It is not surprising that a bridge is being built between veterinary medicine and humans. You shouldn’t forget that about 70 percent of pathogens in humans originally come from animals. We see that the “cross health” or “one health” principle is on the rise. That principle brings veterinary and human medicine together to discover solutions.”
“Under the influence of climate change and globalization, there are a number of pathogens that are shifting or increasing their range. One health is increasingly seen as the way to work to get diseases under control,” Eric Cox concludes.
Read more articles on vaccine research at Ghent University on Dare To Think.
Read also
Five (realistic) ways to move more in 2026
January often starts with good intentions… but those plans can be quickly abandoned. To exercise more is always high up everyone’s list, but there’s often a gap between wanting to do it and actually doing it. So how do you bridge that gap?
Is a stool transplant a potential treatment for Parkinson’s?
A recent study into Parkinson’s disease has shown that a stool transplant may constitute a new and valuable treatment of the disease. “It offers a potentially safe, effective and cost-efficient way of alleviating the symptoms and improving the quality of life of millions. A 'bacterial pill' might replace the stool transplant in the future. But more research is needed.”
Ignaas Devisch has been stimulating our thinking for years (and is now receiving recognition for it)
Twenty years ago, he was ridiculed as a scientist when he tried to communicate with the general public. Now, Ignaas Devisch is receiving the Science Communication Career Award for it. "It's wonderful recognition," says the medical philosopher. "Although communicating about science also involves learning to listen well."
‘Women are not just copies of men with breasts and ovaries.’
Van wetenschappelijk onderzoek tot medische behandelingen, decennialang stond de man centraal in de medische wereld. Betekent dat dan ook dat vrouwen daardoor minder goede zorg krijgen?



